Medical Exercise CPT & ICD-10 Codes in 30 Minutes
Unlock Insurance Reimbursement: A Guide to CPT & ICD-10 Codes for Medical Exercise Professionals
Good morning! Michael Jones from the Medical Exercise Training Institute here, and welcome to a crucial discussion for all medical exercise professionals looking to expand their practices and connect with the medical community: CPT and ICD-10 codes.
For years, the idea of insurance reimbursement for medical exercise professionals seemed like a distant dream. However, I'm happy to say that we are increasingly seeing medical exercise professionals successfully navigate the world of insurance carriers and receive reimbursement for their valuable services, especially over the last decade.
This brings us to the core of our discussion: understanding ICD-10 codes, the diagnostic codes, and CPT codes, the current procedural terminology codes, which are essential when dealing with insurance carriers. But let me be absolutely clear: simply knowing a CPT code is not the answer. There is a systematic process involved in submitting insurance claims for reimbursement for medical exercise training services.
For those unfamiliar, the Medical Exercise Training Institute has been at the forefront of this field for 31 years, starting with our first medical exercise specialist workshop and certification. We recognized the need to provide education and training to help medical exercise professionals effectively transition clients from physical therapy clinics into safe and effective exercise programs, especially as insurance cutbacks in the 1990s led to earlier patient discharges. Now, we're seeing more and more of our members become providers within insurance networks or receive reimbursement from insurance carriers.
So, what do you, as a medical exercise professional, absolutely need to know about CPT and ICD-10 codes? Let's break down the key points:
Understanding Your Scope of Practice is Paramount
Before even thinking about billing, you must have a firm grasp on your scope of practice as a medical exercise specialist. You can bill for services within this scope, which includes:
- Medical exercise training or ME assessment
- Cardiovascular training
- Flexibility training
- Strength training
- Functional conditioning
- Back training
- Lifestyle education
- Aquatic training
- Stabilization training
It's crucial to note what falls outside your scope of practice as a non-licensed provider. You cannot bill for procedures performed by licensed medical professionals like physical therapists, chiropractors, occupational therapists, nurses, or physicians. Your role involves managing medical conditions through exercise after other therapies are completed and with a referral. Always be upfront with clients, referring medical professionals, and insurance carriers about your role and credentials.
Key Reimbursement Criteria to Consider
Not every client with a medical condition can have their workouts billed to insurance. Here are the essential criteria for reimbursement:
- Written Referral: You must have a written referral from an MD, DO, DPM, NP, or PA. The referral should specify "medical exercise training," "functional conditioning," or "post-rehab training" and should not mention "personal training" or any form of therapy (physical therapy, exercise therapy).
- Maximum Benefit from Therapy: The client should have received maximum benefit from physical therapy, occupational therapy, or chiropractic services before starting with you.
- Chronic Conditions or Residual Deficits: The client typically has a chronic condition, has undergone surgery, or has residual functional deficits from their injury, surgery, or condition. This is not for acute injuries where medical care is ongoing.
- Insurance Coverage Limitations: Insurance coverage should not be via Medicaid or Medicare, as their guidelines typically require the provider to be a licensed medical professional.
Navigating CPT Codes: The Procedures You Can Bill For
CPT codes describe the specific procedures you perform. Here are some of the most commonly used codes for medical exercise training:
- 97110 - Therapeutic Exercise: This covers basic exercises focused on increasing strength, flexibility, endurance, and balance.
- 97112 - Neuromuscular Re-education: This code is used for higher-level exercises focusing on balance, coordination, posture, standing, and gait. While 97116 (Gait Training) exists, 97112 often encompasses many gait-related activities. It's advised to use 97116 sparingly.
- 97530 - Therapeutic Activities: This code applies when utilizing activities or exercises geared towards the client's functional capabilities, such as reaching, bending, sitting, getting out of a chair, lifting, pushing, and activities of daily living.
- 97535 - Self-Care/Home Management: Used when assisting a client with setting up their home or navigating their living environment, focusing on lifestyle management.
- 97750 - Physical Performance Testing: Can be used for functional assessments with measurement tools like the weight and balance scale.
- 97161 - Low Complexity Assessment/Evaluation: Often the best way to bill for the initial client evaluation.
Remember, these codes are typically billed in 15-minute increments, although insurance carriers are increasingly scrutinizing and considering 8-minute increments. If a session lasts 45 minutes, you would generally use three of these codes. It's recommended to vary the codes to accurately reflect the services provided during the session, rather than using the same code multiple times.
Understanding ICD-10 Codes: The Necessary Diagnoses
CPT codes alone are insufficient. Every insurance claim requires a diagnostic code, and all diagnoses fall under the ICD-10 coding system. These codes explain why the client requires your services. Your ICD-10 codes must logically align with the CPT codes you are using. For example, billing for exercise with a diagnosis of a sinus infection (without any related mobility issues) will likely result in a claim rejection.
Here are a few examples of ICD-10 codes relevant to the musculoskeletal, neurological, and cardiovascular/metabolic realms:
- Musculoskeletal: M17.9 (Osteoarthritis of the knee), M16.9 (Osteoarthritis of the hip), M47.812 (Spondylosis without myelopathy or radiculopathy in the cervical spine), M51.26 (Intervertebral disc displacement in the lumbar spine), M54.5 (Low back pain), M79.7 (Fibromyalgia)
- Neurological: G20 (Parkinson's disease), G35 (Multiple sclerosis), G81.90 (Hemiplegia)
- Cardiovascular/Metabolic: I10 (Essential hypertension/high blood pressure), E11.9 (Diabetes type 2 without complications/high blood sugar), E66.9 (Obesity)
- Other Relevant Codes: Z91.81 (History of falling), R26.89 (Abnormalities with gait or mobility), Z98.89 (Postsurgical condition), Z47.1 (Aftercare following total joint replacement), Z96.651 (Presence of right artificial knee joint)
It is crucial to obtain the primary and secondary ICD-10 codes from the referring physician or their office. These codes must support the medical necessity of the medical exercise training you provide.
The Codes Must Align: Ensuring Successful Reimbursement
The connection between the ICD-10 diagnosis and the CPT procedure is vital. The ICD-10 code should justify the use of the specific CPT codes you are billing for. A mismatch will likely lead to insurance claim rejection. Furthermore, the written referral from the physician must also support the CPT and ICD-10 codes you are using.
Ready to Crack the Code to Insurance Reimbursement?
Understanding CPT and ICD-10 codes is a significant step towards successfully billing insurance for your medical exercise training services. Remember, it's not just about knowing the codes, but also about understanding your scope of practice, meeting the reimbursement criteria, ensuring proper documentation, and following a systematic process.
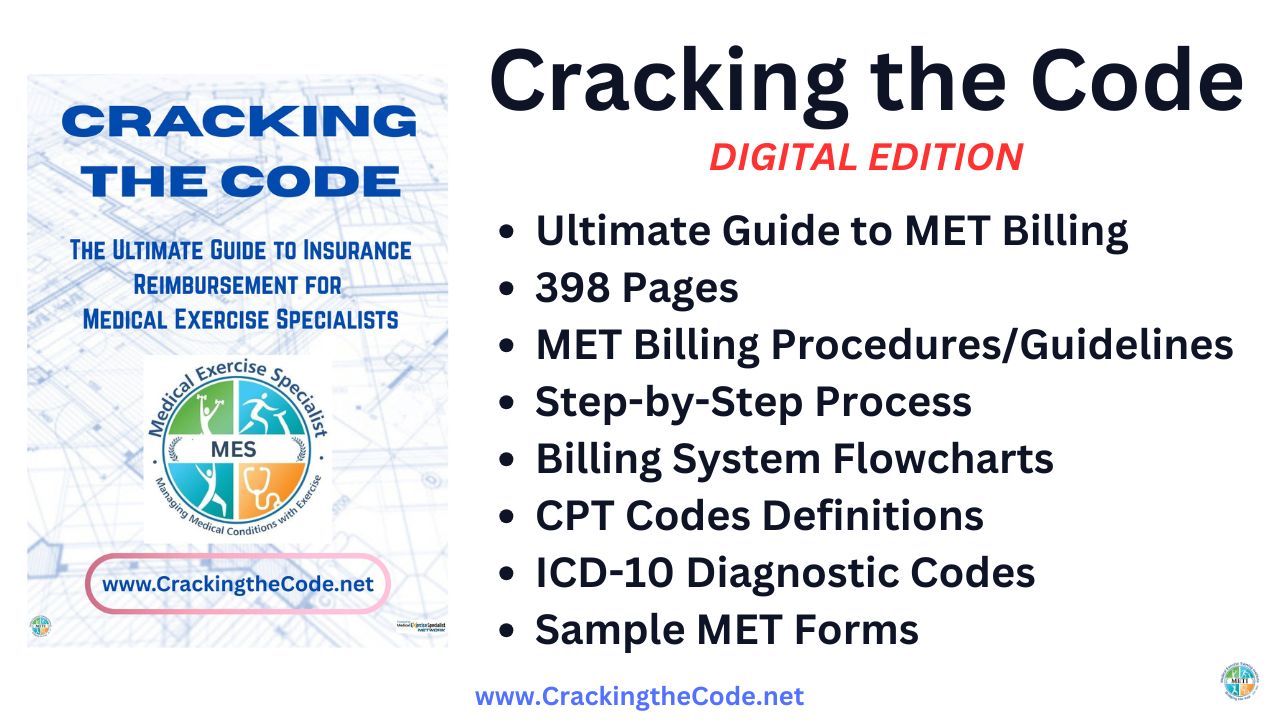
To gain a comprehensive understanding of this process, including step-by-step guidelines, billing systems, sample forms, and much more, we encourage you to visit CrackingtheCode.net to purchase our "Cracking the Code - The Ultimate Guide for Insurance Reimbursement for Medical Exercise Specialists" manual. This 398-page manual contains everything a medical exercise professional needs to navigate insurance reimbursement.
At CrackingtheCode.net, you can also find recordings of past webinars that delve deeper into these crucial topics. Don't miss out on this invaluable resource to help you build your practice and better serve your clients!
Click the Image to Get Your Copy - Only $129 (Immediate Download)
Get Medical Exercise Training guidelines and updates!
Build your practice with tips learned over 28+ years teaching MedXPROs around the world!!